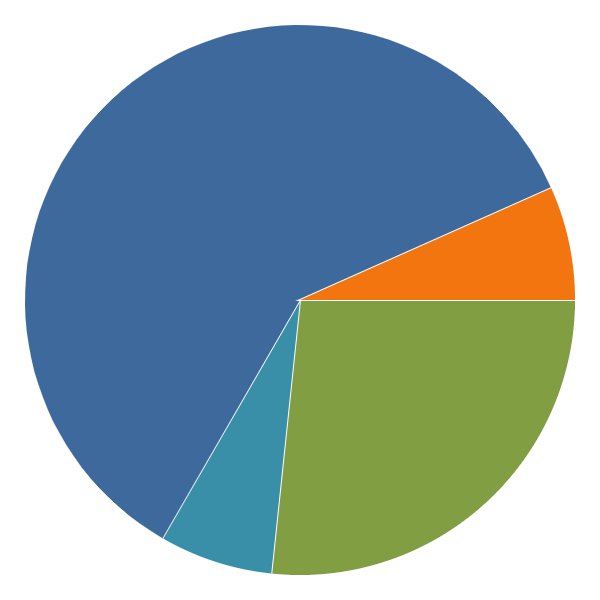
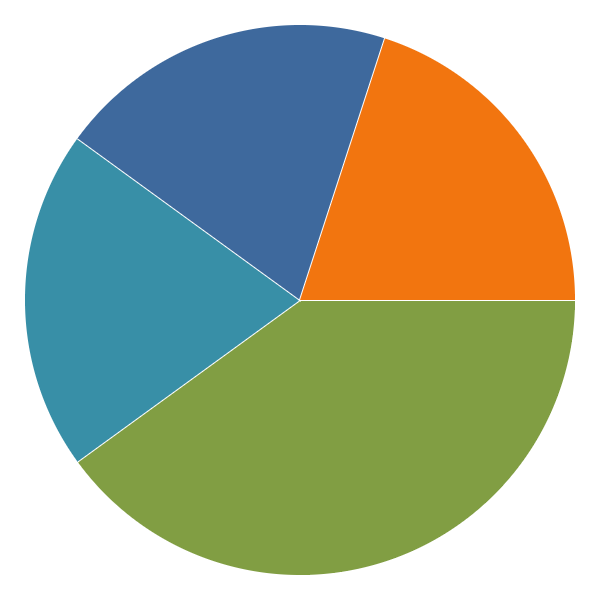
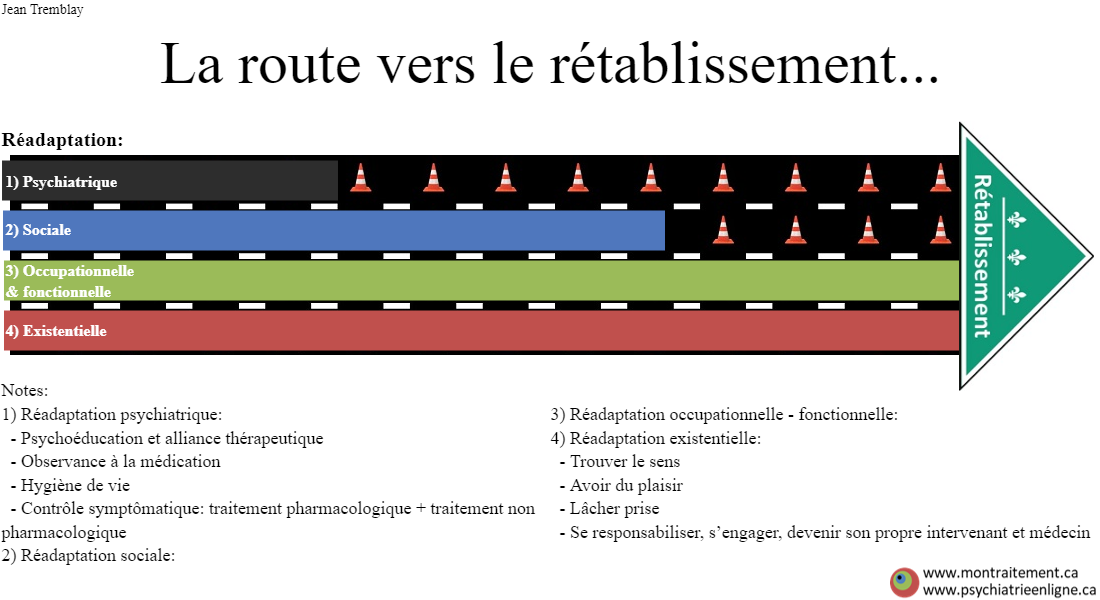
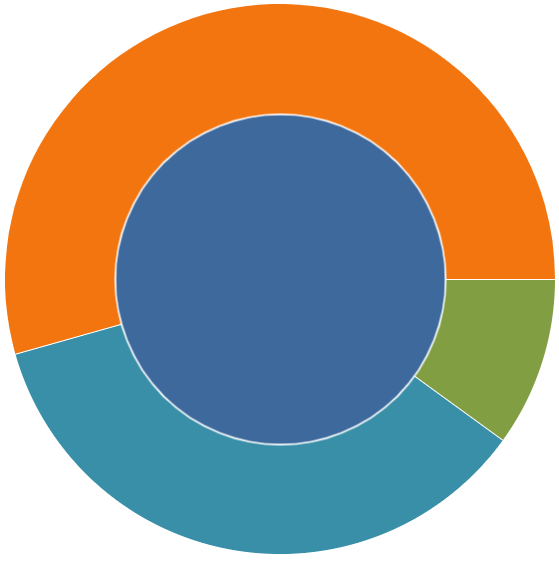
Pie chart App of the “4 Pillars Model”
Description:
This tool allows clinicians to quickly represent in proportions the holistic model of care integrated to the person. It is a reminder that care cannot be solely pharmacological. Rather, health and wellness are complex concepts so that treatment cannot be reductionist either. By sliding the gradators, we represent the person’s current or expected care in terms of: 1) Support, 2) Lifestyle, 3) Medication, 4) Attitude and psychological strategies. As 100% is the totality of care, each patient gets to decide how much to invest in the different dimensions of care in order to achieve his or her care and life goals. Obviously, these proportions can vary with time, the patient’s progress, clinical and psychosocial reality, learning, unforeseen events, redefinition of objectives… The “diagnosis” of the current situation encourages discussion of future treatments and especially of the role and commitment expected from the patient in his or her care. The “4 Pillar model” is also named the “4P model”: Pharmacotherapy, Psychotherapy, Philosophy, Practice (lifestyle, social support, administrative support, problem solving…). This less common formulation is more useful for clinicians in describing and organizing their interventions.
Exemple:
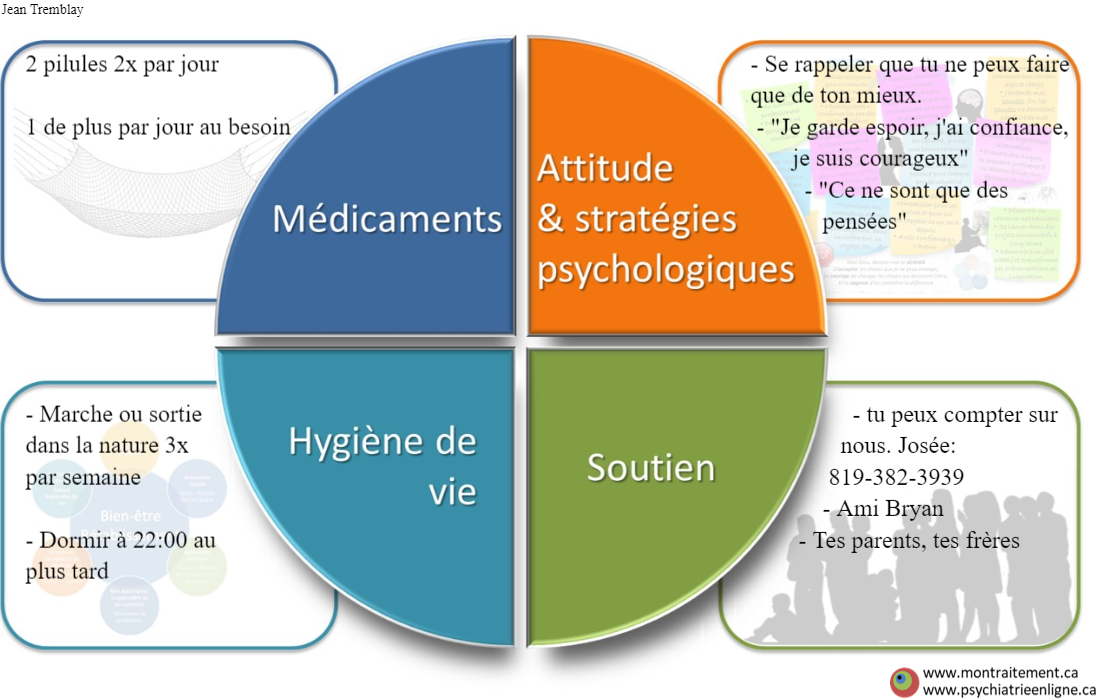
Personalized and Simplified Recovery Plan (PR2) based on the “4 Pillars Model”
Patients often forget the different aspects of the treatment discussed and proposed during the meeting with the physician or practitioner. Typically, they only remember the pharmacological change proposed and written on the prescription. This tool provides a global view of the holistic care to remind patients of the current care plan or recovery plan (RP) in terms of 1) Support, 2) Lifestyle, 3) Medication, 4) Attitude and psychological strategies. The image produced by this tool becomes a “bio-psycho-social-responsibility care prescription”, a reminder that one can benefit from care (“passive care”), but should also activate and self-impose duties/responsibilities to achieve his/her wellness (“active care”). Ideally, the process is co-designed with the physician or caregiver for a co-creation of the plan that promotes shared decision making and thus engagement of the patients in their responsibilities towards their wellness. This image becomes a basis for future discussions and follow-ups so that continuity of care is promoted. It becomes a simplified and accessible recovery plan (RP) “at a glance” that the patient and his or her caregivers can constantly refer to in order to be engaged in actions towards his or her wellness. A plan gives birth to hope.
In this model, medication is seen as a “pharmacological safety net”, a “pharmacological crutch” to support all other aspects of care. This is also commonly a person’s view of the chemistry they ingest through their medication. They hope to use it only temporarily, as it is the case with most pharmacological treatments in somatic care (i.e., antibiotic therapy). This is an opportunity to support the person in adopting other non-pharmacological means of treatment “to compensate” for the reduction and perhaps even the eventual cessation of this crutch. The 4Ps model thus helps with the discussion, “negotiation” and empowerment of the person in their recovery process. In the early care situation for psychosis – and probably for many other conditions – medication is seen as an “adjunct” to care, while therapy and other non-pharmacological elements of care are seen as the “essential and indispensable” ingredients for recovery. As an analogy, the crutch/cast is very helpful following a leg fracture, but it is the physical therapy and the person’s efforts that allow him/her to recondition, to walk… At the clinic, we often need to be explicit about the expectations of medication so that the “proposed crutch remains a pillar and not a burden. (PPv2.0 page: T5)
source: The PR2 model was presented at Journées annuelles de santé mentale JASM 2019 “Les multiples facettes d’une intégration prometteuse” – May 7th 2019 by MSSS (https://www.msss.gouv.qc.ca/professionnels/documents/journees-annuelles-de-sante-mentale/A7_PR2_JASM%202019_Dr_Tin_Ngo-Minh_2019.pdf)
Example
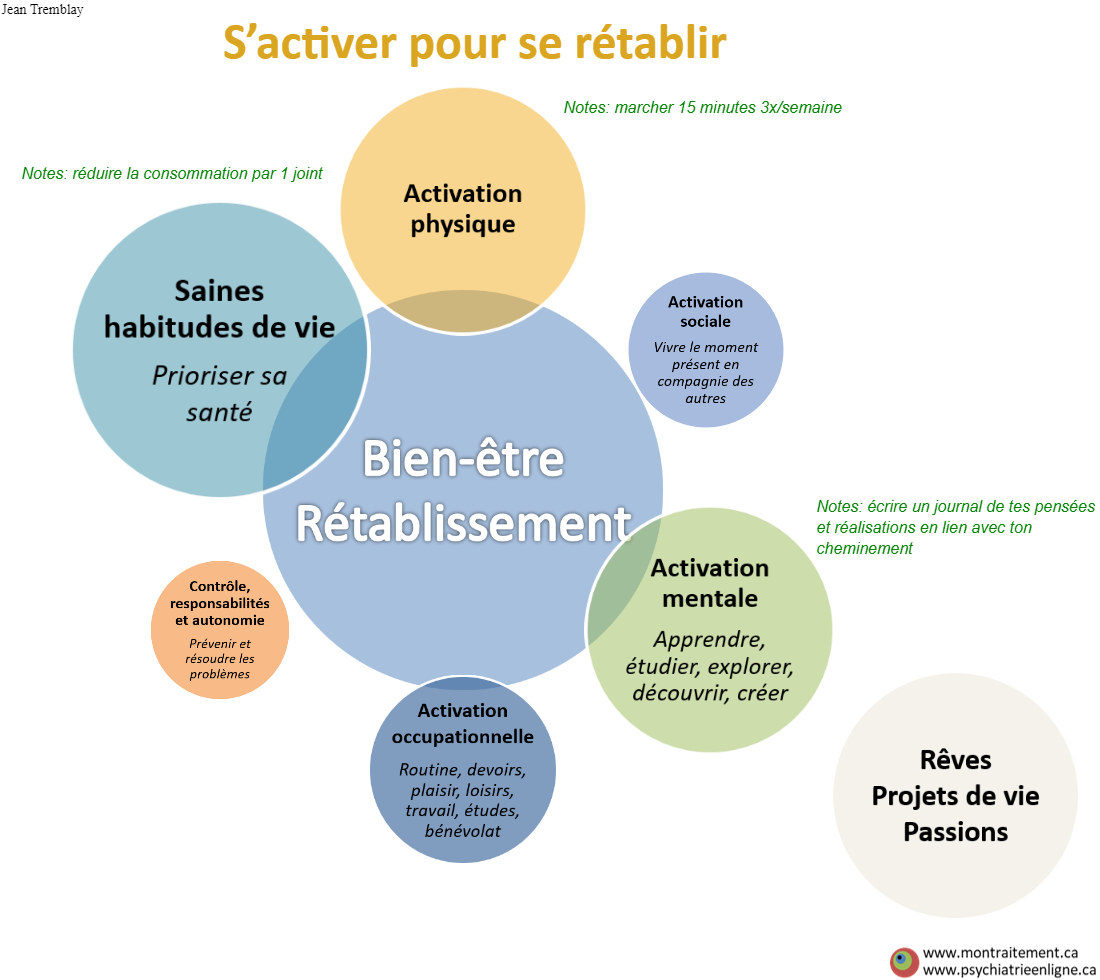
The Flower of Healthy Living
Description:
One often considers him/herself as a recipient of care, a person who expects services that are owed to them. This psychology does little to motivate the person’s involvement in his/her care, but rather places one in a “victim” position in front of a health care system that is often not accessible or too slow to give them what they say they are entitled to: psychotherapy, support from a social worker, occupational therapy, etc. This is a detailed prescription for healthy living, the 4th pillar of PR2: physical activation, social activation, mental activation, occupational activation, taking responsibility for one’s life and healthy lifestyle habits. You have to be active to get well. The image produced by the tool becomes a prescription, containing the duties for well-being. It is therefore an extension of the recovery plan (PR2) that is previously described, where the “non-pharmacological aspects of treatment” are emphasized, for which the patient in question is primarily responsible. He/she can no longer rely on the excuse of being “waiting for services/care”. It proposes concrete, tangible and achievable care (i.e. SMART goals). The person has a plan, knows he/she has control, knows what can be done for his/her well-being. A plan gives birth to hope. This tool promotes the concept of self-care, a rational self-care. It is probably the most widely used tool/image in practice at the clinic. Our experience is that this image allows for better follow-up, the establishment of “healthy expectations” from the physician or caregiver towards the person and vice versa. Indeed, the tool promites a therapeutic discussion/negotiation: “here is what you have to do… here is what I, on my side, will have to do in return (reduce medication, follow-up, etc…)”. (PPv2.0 page: T7)
Example:
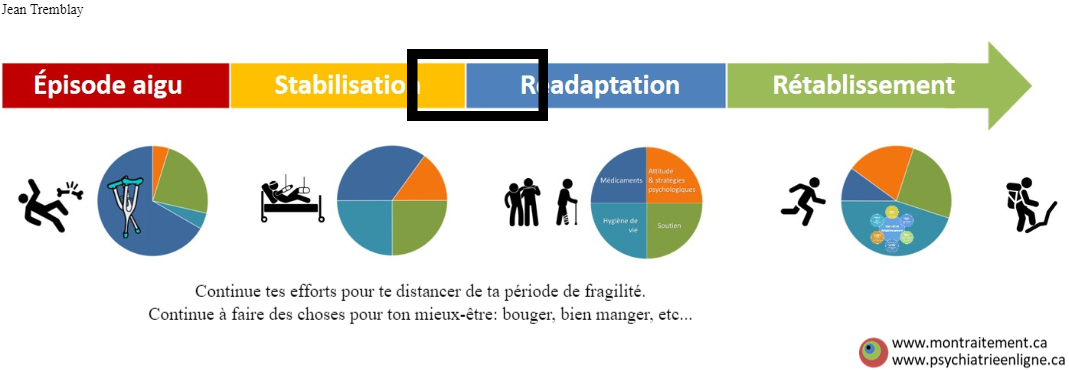
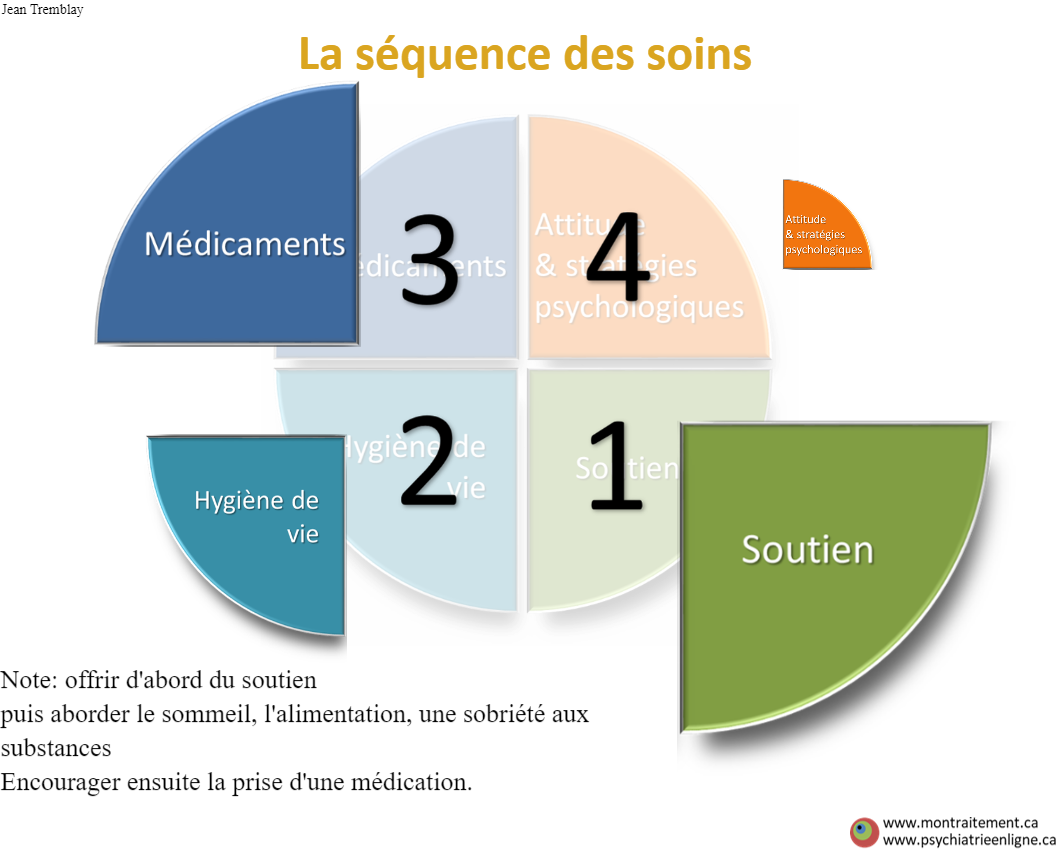
Situated Oneself In the Sequence of Care 1
Description:
Being aware of where the person is in his or her treatment journey and knowing the steps ahead can encourage him/her in the present actions towards better health. For the person to know that he/she will likely to have fewer medications and more freedom in the future also promotes hope and engagement in care. One of the weakness of the format of this tool is that it implys the duration of each step being the same, hence we have options of the following other tools. It does, however, serve as a good reminder that the person plays an active role in his or her own well-being and responsibilities to achieve it. It also reminds the clinician that pharmacological treatment should be adjusted and taking up less space as the person becomes more active in their non-pharmacological care towards their well-being. (PPv2.0 page: T6)
Example:
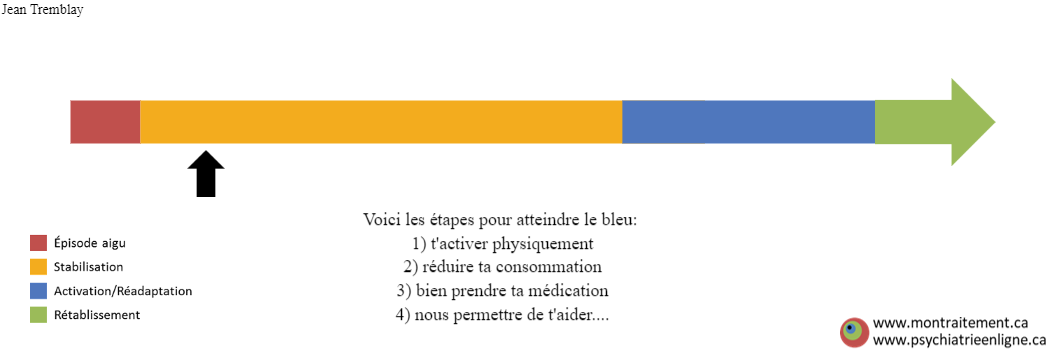
Situated Oneself In the Sequence of Care 2
Description:
Knowing where the person is in his or her treatment journey and knowing the steps ahead can encourage him/her in the present actions towards better health. For one to know that he/she will likely to have less medication and more freedom in the future also promotes hope and engagement in care. This tool addresses the shortcoming of the previous tool in that the steps can vary in length. (PPv2.0 page: T6)
Exemple:
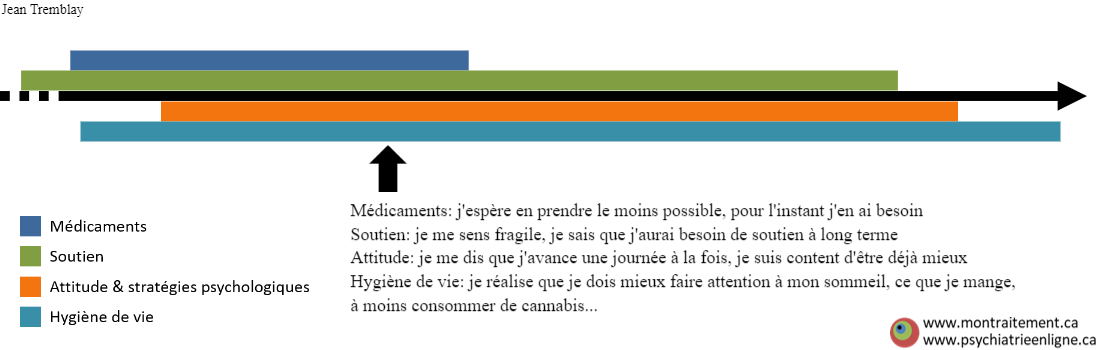
Personnalize the Sequence of Care 1
Description:
The path to recovery is different for each person, so are the ingredients. Knowing where the person is in his/her therapeutic journey and knowing the current or desired ingredients of care encourages one in the present and future actions towards well-being. This chart also encourages patients because it reminds them of their goal of no further follow-up or care, which is shared with the treatment team. As patients adjusts things in their life, adopt a healthier lifestyle, take on better ways of managing stress, they require less social/administrative and/or pharmacological support. The timing of care and the dose of each ingredient should be personalized to make treatment meaningful and to encourage patient commitment. This tool is a reminder that multiple care/actions are needed concurrently and not only sequentially in the recovery process.
Exemple:
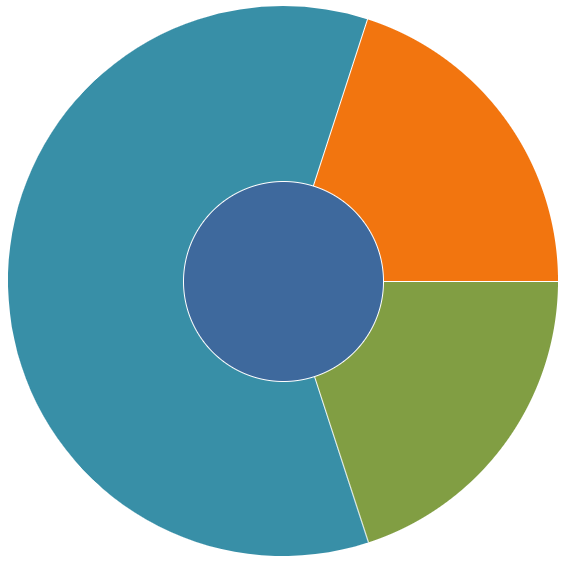
Personnalize the Sequence of Care 2: the Path towards Recovery
Description:
There are several dimensions of rehabilitation that need to be concurrently considered : psychiatric rehabilitation, social rehabilitation, occupational/functional rehabilitation, existential/spiritual rehabilitation, not to mention physical rehabilitation, which is not typically addressed at the beginning of a person’s care at FPE. Knowing where the person is in their therapeutic journey and knowing the current or desired ingredients of care can encourage him/her in the present and future actions towards personal well-being. This chart also encourages patients because it reminds them of their goal of no further follow-up or care, which is shared with the treatment team. As patients adjust things in their life, adopt a healthier lifestyle, take on better ways of managing stress, they require less social/administrative support and/or pharmacological support. Knowing that there is “an end, a destination” to this road can be a relief to people especially if they feel stuck early on in their treatment and can’t see the end. The tool is also reflecting the roads of Quebec Health System and its pitfalls…
Exemple:
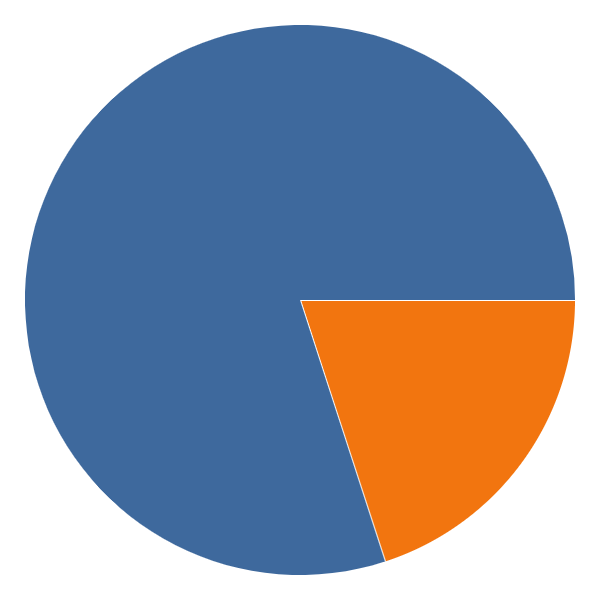
Biopsychosocial approach to care vs. classical dichotomous bio vs. psychosocial approach
Description:
Classically, care was offered in a siloed and clearly dichotomous way: pharmacological care vs. non-pharmacological care, without any integration. This tool allows for a better visualization of the person/caregiver’s current or desired investment in each of these two dimensions of care. This graph is sometimes more useful and also simpler to understand compared to the “Piechart of the 4 Pillars Model” tool when focusing on only 2 overall sets of care: “pharmacological treatment”, the medication and “non-pharmacological treatment”, the psychosocial. Some people hope that medication will solve their difficulties, others the opposite. The ideal is to personalize the care and to constantly adjust it according to the person’s evolution. In general, however, the reality often involves a combination of several pharmacological and non-pharmacological treatments.
Exemple:
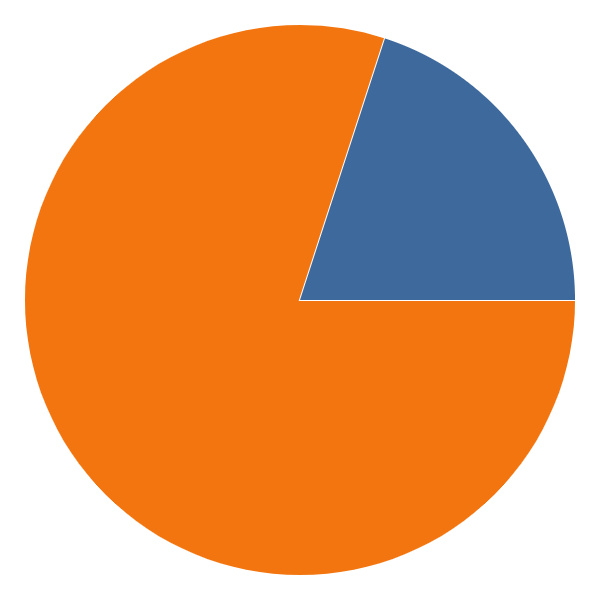
Integrated biopsychosocial approach to care with a Central Primary Treatment
Description:
This is another schematic of the “4 Pillars Model” to represent holistic biopsychosocial care. The 4-pieces-of-the-pie layout of the “4-pillar model” suggests the concurrent introduction of all pharmacological and non-pharmacological elements of care at the very beginning of care. In reality, care rarely begins with all biopsychosocial elements. Usually, the initial dominant treatment is pharmacotherapy, since care often begins at an acute episode requiring rapid stabilization, where medication has its main place. Thus, this diagram helps to better describe the primacy of a particular care in the management of the patient. This initial care often has a catalytic effect in the implementation of other therapeutic dimensions. Pharmacotherapy is thus, in our view, in the service of other psychosocial therapeutic elements. This chart serves primarily to explain this nuance of the biopsychosocial model of care to health care professionals, although the “4 pillar model” with 4 quarters of pie remains a more practical way of presenting holistic care to patients.
Exemple: